
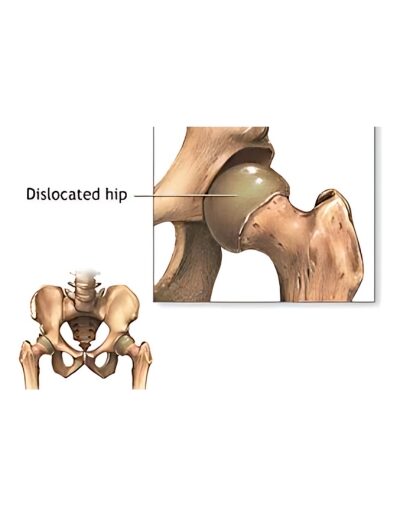

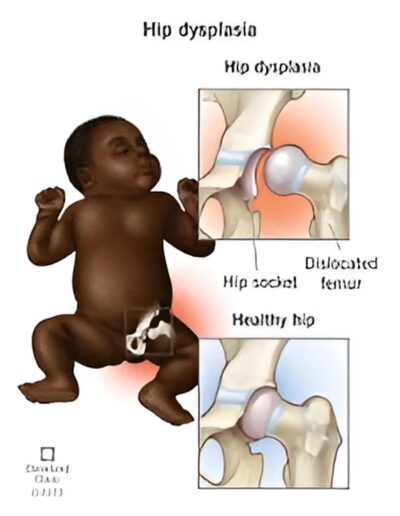
Developmental dysplasia of the hip (DDH or hip dysplasia) is a relatively common condition in the developing hip joint. It occurs once in every 1,000 live births. The hip joint is made up of a ball (femur) and socket (acetabulum) joint. In DDH, this joint may be unstable with the ball slipping in and out of the socket.
In addition, the socket is often shallow which can increase a person’s risk of developing arthritis and joint pain later in life. Hip dysplasia has wide spectrum of severity ranging from a mildly shallow hip socket to a completely dislocated hip.
The greatest incidence of DDH occurs in first-born females with a history of a close relative with the condition and/or history of breech position in utero.
The exact cause(s) of hip dysplasia are unknown, but it is likely that many factors both environmental and genetic play a role.
One of the environmental influences thought to contribute to hip dysplasia is the baby’s response to the mother’s hormones during pregnancy. A tight uterus that prevents fetal movement or breech position may also cause hip dysplasia. The left hip is involved more frequently than the right due to intrauterine positioning.
Another environmental factor is infant positioning in the first year of life. Cultures that hold infants wrapped around a caregiver such that the hips are held apart generally have lower rates of DDH. In contrast, cultures which typically swaddle or papoose an infant with the hips extended have high rates of hip dysplasia.
First-born babies are at higher risk since the uterus is small and there is limited room for the baby to move; therefore affecting the development of the hip.
Other risk factors may include the following:
Specific treatment for DDH will be determined by your baby’s physician based on:
The goal of treatment is to put the femoral head back into the socket of the hip and to deepen the socket so that the hip can develop normally. Treatment options vary for babies and may include:
The Pavlik harness is used on babies up to 6 months of age to guide the hip into place, while allowing the legs to move a little. The harness is put on by your baby’s physician and is usually worn full time for several weeks, then part-time for an additional number of weeks.
Your baby is seen frequently during this time so that the harness may be checked for proper fit and to examine the hip. During the course of treatment, ultrasound (or x-ray) will be used to check hip placement and the development of the socket.
Most hips in infants can be successfully treated with the Pavlik harness, but sometimes, they may continue to be partially or completely dislocated.
If the hip continues to be partially or completely dislocated, the second line of treatment is an abduction brace, which is more rigid and can be used beyond 6 months of age in older and bigger infants.
These braces generally allow less motion than a Pavlik harness and are therefore more restrictive but can be quite successful for those infants in whom the Pavlik does not work.
If the harness and/or brace are not successful, a procedure under anesthesia may be required to put the hip back into place manually, also known as a closed reduction. If successful, a custom molded body cast (called a spica cast) is put on the baby to hold the hip in place. The hip spica cast is usually applied from the chest down to the ankle of the affected side and usually includes part of the opposite leg as well.
The spica cast is worn for approximately three to six months. The cast is changed from time to time to accommodate the baby’s growth and for hygiene reasons. Following casting, a brace and/or physical therapy may be necessary to promote deepening of the hip socket and strengthen the muscles.
Cardiology is the medical specialty that deals with the diagnosis and treatment of diseases related to the heart and blood vessels. Basic knowledge of cardiology includes understanding the anatomy and function of the heart, the various cardiovascular diseases, risk factors for heart disease, diagnostic techniques such as electrocardiograms (ECGs) and echocardiograms, treatment options including medications, interventions, and surgeries, and preventive measures to maintain heart health.
It is important to note that these symptoms can also be caused by other conditions, and some individuals with heart disease may not experience any symptoms until a more advanced stage. If you are experiencing any concerning symptoms, it is recommended to consult a healthcare professional for a proper evaluation.